Diabetes is a long-term condition affecting how the body processes carbohydrates, fats, and proteins. It is marked by high blood sugar levels and a higher likelihood of heart disease, stroke, kidney issues, and nerve damage. The "mainstream establishment" isn't sure what causes or how to reverse diabetes, but is there more clarity out there?
Diabetes is a long-term condition affecting how the body processes carbohydrates, fats, and proteins. It is marked by high blood sugar levels and a higher likelihood of heart disease, stroke, kidney issues, and nerve damage. When the pancreas doesn't produce sufficient insulin or when cells are resistant to it, blood sugar can't enter cells, resulting in severe complications.
You either "have diabetes" or you're fine: not so
Everything is dependent on a stable blood glucose level concerning diabetes in "modern medicine." The conventional view used to be that you're either fine or you have diabetes as if it were a possession and away to self-identify on an illness. Now we know there's a big grey-area in the middle where someone has a blood sugar problem. If it shoots too high you can become very manic in mood, while if it shoots too low you can become too depressed. The lesson here is very often mood swings are connected with an inability to maintain steady blood glucose levels
Diabetes can be categorized into two main types: type 1 and type 2. Approximately 10% of diabetics fall under type 1, while the remaining 90% are classified as type 2. Type 1 diabetes is characterized by the complete destruction of the beta cells in the pancreas, which are responsible for producing insulin.
Did You Know? We Have Free Email News & Tips
Sign up to the above email list to receive more free updates.
Individuals with type 1 diabetes require lifelong insulin treatment to regulate their blood sugar levels. This type of diabetes occurs when the insulin-producing beta cells are damaged, along with a deficiency in tissue regeneration capacity. In type 1 diabetes, the body's immune system starts attacking the pancreas. Interestingly, about 75% of individuals with type 1 diabetes have antibodies for beta cells, whereas only 0.5 to 2% of non-diabetics possess these antibodies. It is likely that the development of these antibodies is a response to cell damage caused by various mechanisms such as chemical, free radical, viral, or food allergy-related factors. It seems that individuals without diabetes either do not experience such a severe antibody reaction or have a better ability to repair the damage once it occurs.
Types of diabetes: contrary to belief there are 3 types
Type 1
When you have type 1 diabetes, your pancreas doesn't produce enough insulin, which is essential for allowing blood sugar to enter your cells and be used as energy. Without insulin, blood sugar accumulates in the bloodstream, leading to various symptoms and complications associated with diabetes.
Type 2
Did you know that type 2 diabetes occurs when the body struggles to properly regulate and utilize sugar, also known as glucose? This chronic condition causes an excess of sugar to circulate in the bloodstream. Over time, elevated blood sugar levels can give rise to complications in the circulatory, nervous, and immune systems. It's important to manage this condition effectively to maintain overall health and well-being.
Type 3
Type 3 diabetes, also known as Alzheimer's-associated diabetes, is a unique form of diabetes that affects the brain. In this condition, the neurons in the brain lose their ability to properly respond to insulin, a hormone crucial for various cognitive functions such as memory and learning. Many scientists speculate that the decline in insulin levels plays a significant role in the cognitive deterioration observed in Alzheimer's disease.
Major complications of diabetes
- Cardiovascular disease is a serious concern for adults with diabetes, as their risk of death from this condition is significantly higher compared to those without diabetes. In fact, their chances of developing cardiovascular disease are two to four times greater.
- Additionally, it is important to note that approximately 75% of adults with diabetes also have high blood pressure (hypertension), further increasing their risk.
- Another significant complication of diabetes is retinopathy, which is the leading cause of blindness among adults. This highlights the importance of regular eye examinations and proper management of diabetes to prevent vision loss.
- Kidney disease is another major concern for individuals with diabetes, accounting for 43% of new cases requiring dialysis treatment. This emphasizes the need for close monitoring of kidney function and early intervention to prevent further damage.
- Nervous system damage, known as neuropathy, affects a significant percentage of people with diabetes. Approximately 60 to 70% of individuals with diabetes experience mild to severe forms of nerve damage.
- Severe cases of diabetic nerve disease can even lead to lower-extremity amputations, making it crucial to prioritize proper diabetes management and regular check-ups. It is alarming to note that more than 60% of lower-limb amputations in the United States occur among people with diabetes. This highlights the importance of early detection and intervention to prevent such drastic measures.
- Periodontal disease, or severe gum disease, is also prevalent among individuals with diabetes, affecting almost one-third of them. This further emphasizes the need for good oral hygiene practices and regular dental check-ups. Chronic pain is another unfortunate consequence that many diabetics face. Conditions such as arthritis, neuropathy, circulatory insufficiency, or muscle pain (fibromyalgia) can contribute to ongoing pain and discomfort.
- Proper pain management strategies and a multidisciplinary approach to treatment are essential in improving the quality of life for these individuals.
- Depression is a common companion of diabetes, with clinical depression often appearing years before the full onset of diabetes. It can be challenging to treat, especially in individuals with poorly controlled diabetes. Therefore, it is crucial to address both the physical and mental well-being of individuals with diabetes.
- Lastly, autoimmune disorders such as thyroid disease and inflammatory arthritis can further exacerbate the suffering of those with diabetes. This highlights the complex nature of the condition and the need for comprehensive care to manage all aspects of the disease.
Overall, it is evident that diabetes can have far-reaching effects on various aspects of a person's health. Proper management, regular check-ups, and a holistic approach to
Please donate to the "Pay It Forward" Campaign
This donation will help others obtain individualized help who can't afford it.
Nowadays, type 2 diabetes is no longer limited to overweight individuals over the age of 40.
It has become a concerning issue even among children, thanks to the widespread obesity epidemic affecting people of all ages in America. Additionally, exposure to high levels of persistent organic pollutants (POPs) has also contributed to the rise of this disease.
At the start, type 2 diabetes often sees high insulin levels, signaling a reduced sensitivity to insulin in the body's cells. Obesity plays a significant role in this decreased sensitivity. Around 90% of those with type 2 are considered obese. However, reaching a healthy body weight can lead to a return to normal blood sugar levels for many patients. Even if insulin deficiency has developed, shedding excess weight usually leads to substantial enhancements in blood sugar management and a significant decrease in risks like cardiovascular disease.
Type 2 diabetes is a condition where blood sugar control deteriorates over time. It typically begins with slight changes in post-meal glucose levels, then progresses to higher fasting plasma glucose levels, and may eventually result in insulin deficiency, requiring insulin treatment.
Other types of diabetes
African-Americans, Hispanic/Latino-Americans, and American Indians are at a higher risk of developing a relatively unknown "gestational diabetes." Additionally, obese women and those with a family history of diabetes are more prone to this condition. Following pregnancy, 5 to 10% of women with gestational diabetes may develop type 2 diabetes, with the risk increasing to 20 to 50% within 5 to 10 years post-pregnancy.
Prediabetes, also known as impaired glucose tolerance, is characterized by having a fasting glucose level of 100–125 mg/dl and/or a postprandial glucose level of 140–199 mg/dl. This condition serves as the initial stage of insulin resistance and affects approximately 57 million Americans. Despite being reversible in most cases, many individuals with prediabetes will eventually develop full-blown type 2 diabetes. However, through making dietary and lifestyle changes, it is possible to completely avoid the onset of diabetes. Several factors contribute to the development of prediabetes, insulin resistance, and the progression to type 2 diabetes.
These factors include consuming a diet high in refined carbohydrates, especially high-fructose corn syrup, having a high intake of saturated fats, overeating due to larger portion sizes, experiencing an increase in inflammatory markers, lack of physical activity, exposure to industrial pollution, gaining weight in the abdominal area, hormonal imbalances, inadequate sleep, and nutrient deficiencies.
New research findings have revealed that people who present with prediabetes face a greater susceptibility to cardiovascular disease (CVD). Additionally, a significant number of individuals with prediabetes display symptoms of metabolic syndrome, which is a collection of factors that substantially increase the likelihood of developing CVD and type 2 diabetes.
Here are some factors to consider when assessing your health: 1. A higher waist-to-hip ratio 2. Two of the following indicators: - Triglyceride levels exceeding 150 mg/dl - Low HDL levels (less than 40 mg/dl for men, less than 50 mg/dl for women) - Elevated blood pressure (above 130/85 mm Hg) - Fasting blood glucose levels above 100 mg/dl.
According to the Third National Health and Nutrition Examination Survey (NHANES III), the prevalence of metabolic syndrome in the United States is 39% among men and women over the age of 20. Among adolescents, approximately 5.8% meet the criteria for metabolic syndrome. It is important to note that individuals with metabolic syndrome not only face a higher risk of cardiovascular disease and diabetes but also experience a lower quality of life, both physically and mentally.
The typical signs of type 1 include increased urination, sudden weight loss, slow wound healing, infections, and constant thirst and hunger. On the other hand, type 2 symptoms are usually less severe, making them easy to miss. This is why a lot of individuals with type 2 are unaware of their condition. Excessive belly fat, fatigue, vision problems, delayed wound healing, gum disease, and recurrent infections are common indicators of type 2.
Diagnosing diabetes: standard is usually using "snap shot in time" blood tests but these have severe limitations
Diagnosing diabetes typically involves measuring blood glucose levels. The first measurement is usually taken after fasting for at least 10 hours but no more than 16. A normal reading falls between 70 and 99 mg/dl. If a person consistently has a fasting blood glucose level greater than 126 mg/dl (7 mmol/L) on two separate occasions, they are diagnosed with diabetes. On the other hand, a fasting glucose level between 100 and 126 mg/dl is categorized as prediabetes.
Determining postprandial and random glucose levels can be incredibly useful in diagnosing diabetes. A postprandial measurement is typically taken one to two hours after a meal, while a random measurement can be taken at any time during the day, regardless of the last meal. If the reading exceeds 200 mg/dl (11 mmol/l), it is considered a strong indication of diabetes..
Type 1 Diabetes: Causes
In type 1 diabetes, the insulin-producing cells in the pancreas are destroyed, usually by the body's own immune system. However, what triggers this destruction can vary from person to person. Genetic factors may make the insulin-producing cells more vulnerable to damage, either due to impaired defense mechanisms, an oversensitive immune system, or a defect in tissue regeneration. These genetic factors, known as "susceptibility genes," modify the risk of diabetes but are not the sole cause of the disease. Instead, they create a foundation for environmental or dietary factors to initiate the destructive process. The term "predisposition" clearly suggests that something else needs to happen, as less than 10% of those with a genetic susceptibility actually develop type 1 diabetes.
In extensive research, it was found that the likelihood of both identical twins developing type 1 diabetes was only 23% in one study8 and 38% in another study9. However, if one twin develops type 1 diabetes after the age of 24, the chances of the second twin developing it drop significantly to just 6%. These findings, along with other studies, suggest that environmental and dietary factors play a more significant role than genetic predisposition in most cases.
There is compelling evidence that highlights the importance of focusing on dietary and environmental triggers
- The number of people diagnosed with type 1 diabetes worldwide has increased significantly, by three to ten times, in the last 40 years. This surge cannot be solely attributed to genetic predisposition, as genetic changes across populations take much longer to manifest.
- Moreover, the rate of type 1 diabetes can skyrocket when individuals from regions with low prevalence move to developed countries. For instance, the rate of type 1 diabetes spiked by almost four times in Asian children relocating to Great Britain and over seven times in Polynesians migrating to New Zealand within a decade. These rapid changes cannot be explained by genetics alone.
- Additionally, there is a notable link between maternal vitamin D levels and the risk of a child developing type 1 diabetes.
Early intervention & possible reversal of Type 1
Intervening early in type 1 diabetes to target the autoimmune or oxidative process could potentially extend the "honeymoon" phase (the period before insulin is crucial) or even reverse the damage altogether. Niacinamide and epicatechin are two substances that might offer some advantages in this area.
Niacinamide
Studies have demonstrated that vitamin B3 in the form of niacinamide can effectively shield pancreatic beta cells from immune-mediated destruction and even potentially reverse the damage caused. This promising finding prompted researchers to conduct pilot clinical trials, which initially supported these observations. Furthermore, these trials indicated that if administered promptly after the onset of diabetes, niacinamide could potentially aid in the restoration or preservation of beta cells, thus slowing down their destruction.
Epicatechin
Epicatechin, the second natural compound with potential benefits, has sparked interest in recent-onset type 1 diabetes research. Scientists initially explored the bark of the Malabar kino tree, a botanical medicine widely used in India to treat diabetes. Extracting epicatechin from the bark revealed its ability to protect beta cells from damage in rats. This discovery holds promise for further investigation into its therapeutic effects.
Factors that Pose Risks to the Environment and Diet
Emerging evidence suggests that issues with the gut's immune system could be a key factor in the immune response against beta cells, leading to the onset of type 1 diabetes. The gut's immune system plays a crucial role in handling various food and microbial antigens to safeguard the body from infections and allergies. In certain instances of type 1 diabetes, it seems that the gastrointestinal immune system produces antibodies that target and harm the beta cells.
It's fascinating to consider the potential impact of poor protein digestion on type 1 diabetes. When dietary proteins are not properly digested, they can interact with proteins present on or within the beta cells of the pancreas. In humans, two specific dietary proteins that could be involved are those found in milk (bovine serum albumin and bovine insulin) and wheat (gluten). For instance, bovine insulin, which differs from human insulin by only three amino acids, can trigger the production of antibodies. If a person develops antibodies to bovine insulin, there's a high likelihood that these antibodies will also attack their own insulin. Apart from causing the destruction of beta cells through antibody-mediated processes, bovine insulin can activate T cells in individuals predisposed to diabetes. This activation can lead to the direct attack and destruction of beta cells by T killer cells.
Viruses, pathogens and diabetes
New research has further supported the idea that type 1 diabetes could potentially stem from a viral infection. The immune system may be getting mixed up on which proteins to target, whether they are from food like dairy or gluten, or similar proteins found on the pancreatic beta cells. This confusion could be linked to a lack of vitamin D. When a person with this confusion gets a viral infection, the immune system goes into overdrive, producing more antibodies and sensitized white cells. These confused immune cells then start attacking the pancreas. Gastrointestinal infections caused by enteroviruses (such as coxsackieviruses and echoviruses) and rotavirus are quite common, particularly in children.
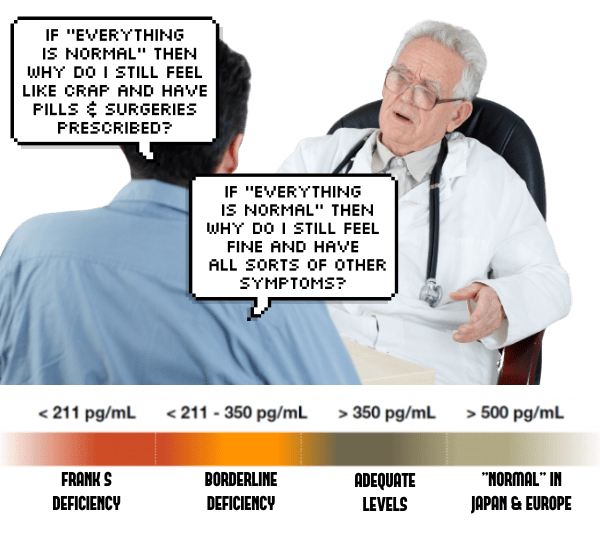
Vitamin D defiency
Research suggests that providing children with vitamin D through cod liver oil and other sources in early childhood may help prevent type 1 diabetes. In a large study conducted in northern Finland, over 12,000 pregnant women were enrolled in 1966, and their children were followed until December 1997. The final analysis of 10,366 participants revealed that kids who consistently consumed vitamin D, mainly from cod liver oil, had an 80% lower chance of developing type 1 diabetes. On the other hand, those with a deficiency in vitamin D had a 300% higher risk of developing the disease.
Omega 3 Fatty Acids & Nitrates
Omega-3 fatty acids have been shown to have a positive impact on reducing the risk of type 1 diabetes in various studies. Essential fatty acids have been found to delay the onset of type 1 diabetes, while higher levels of omega-3 in red blood cells are linked to a lower risk. On the other hand, there is a clear connection between increased nitrate levels from food and water and a higher incidence of type 1 diabetes. Nitrates, which are found in fertilizers and processed meats, can lead to the formation of harmful compounds like nitrosamines that are known to contribute to diabetes in animals.
Type 2 Diabetes: causes
Excess body fat, specifically obesity, is the primary risk factor for type 2 diabetes. It's alarming that around 80 to 90% of individuals with type 2 diabetes are obese, with a body mass index greater than 30. When fat cells, especially those around the abdomen, become overloaded with fat, they release various biological molecules like resistin, leptin, tumor necrosis factor, free fatty acids, and cortisol. These molecules hinder the effectiveness of insulin, leading to impaired glucose utilization in skeletal muscle, increased glucose production by the liver, and reduced insulin release by pancreatic beta cells. Another crucial aspect is that as the number and size of fat cells increase, the secretion of compounds that support insulin action, such as adiponectin, diminishes.
Risk factors
If you have a family history of diabetes, such as a parent or sibling with type 2 diabetes, it's important to be aware of the increased risk. Combine that with factors like obesity, an increased waist-to-hip ratio, and age over 45, and the risk becomes even higher. Additionally, certain race/ethnicities, such as African-American, Hispanic-American, Native American/Canadian, Native Australian or New Zealander, Asian-American, and Pacific Islander, may also have an increased risk. If you've previously been identified with impaired fasting glucose or impaired glucose tolerance, or if you've had a history of gestational diabetes or delivered a baby weighing more than 9 lb, it's crucial to take proactive steps to manage your health and reduce the risk of developing diabetes.
Epi-genetics (not solely written in stone 'genetics') of Type 2 Diabetics:
When looking at identical twins, it was found that the concordance rate for type 2 diabetes was between 70 and 90%, indicating a strong genetic link. Family studies further support this, showing that children with one parent with type 2 have an increased risk of diabetes, and if both parents have it, the risk in offspring is nearly 40%. Despite genetic predisposition, most cases of diabetes can still be prevented. Studies on DNA methylation of key genes related to T2D in human pancreatic islets have shown increased methylation and decreased gene expression in diabetic patients compared to non-diabetic individuals.